
RET is a gene and protein involved in controlling cell growth and cell differentiation. Cell differentiation is the developmental process of unspecialized cells growing and changing, becoming specialized, and reaching their mature form and function. RET stands for “rearranged during transfection”, a name that is related to the how the gene was discovered. RET encodes a type of protein called a receptor tyrosine kinase.
RET mutations can cause several cancers, including about 3% of colorectal cancer, as well as non-small cell lung cancer, and more commonly, endocrine cancers like papillary thyroid carcinoma, multiple endocrine neoplasia syndromes, and pheochromocytoma. Genes, like RET, that can cause normal cells to become cancer cells are called oncogenes. Oncogenes can act like an “on switch” for cancer. When the switch changes in the wrong way, it can make cells grow out of control. Oncogene mutations that cause cancer are called oncogenic drivers.
RET mutation is also associated with Hirschsprung’s disease, a non-cancer condition affecting the nerves of the intestine. Hirschsprung’s disease is usually found in babies or young children.
RET fusion happens when part of the RET gene breaks off and attaches to another gene. RET fusion is a kind of abnormality involving a rearrangement of genes. When a piece of a chromosome (the cell structure that carries genes) containing the RET gene breaks off and attaches to a gene on another chromosome, this is called an RET gene fusion. It is a combination of the RET gene and a fusion partner gene.
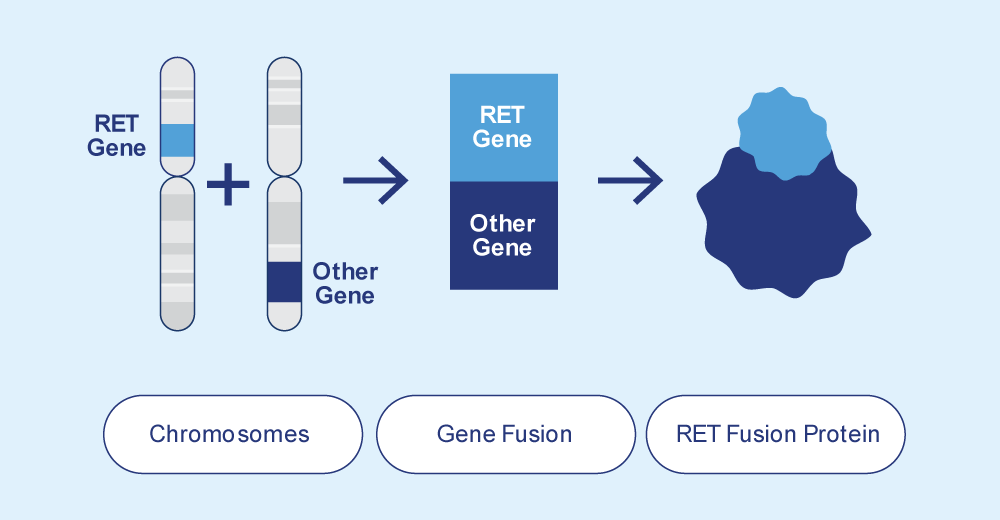
Genes give the instructions for your cells to make proteins, and when RET gene fusion occurs, your cells will make abnormal proteins called RET fusion proteins. RET fusion proteins are a combination of a RET protein and a partner gene protein. Fusion proteins can cause cells to grow and survive when they shouldn’t, leading to cancer.
Colorectal cancers with RET fusion are rare, making up about 1% of CRC, and they tend to have other common biomarker findings.
CRC with RET fusion
The changes in RET that are related to colorectal cancer are not hereditary, meaning they are not passed from parents to children.
RET status is usually tested in a tumor cell biopsy sample. RET abnormalities can be detected with several laboratory methods, including
For the FISH method, probe DNA including the RET gene is created in the laboratory and bound to fluorescent compounds. The fluorescent DNA probe is then added to a sample of tumor DNA. Matching segments of DNA will attach to each other and appear fluorescent. This allows the laboratory to see the similarities and differences in the probe DNA and the tumor DNA.
RET can also be analyzed for mutations in tumor tissue. MET can be tested individually, or as part of a multiple gene panel using next-generation sequencing (NGS). Next-generation sequencing is a method of reading the pattern of many DNA samples at the same time.
If your RET gene has no changes, it may be reported as “RET negative”, “normal”, “wild-type”, “non-mutant”, or “no fusion detected”.
If your RET gene has a mutation, it will be reported as “mutant” or “RET positive”.
If your RET gene has a fusion, it will be reported as “RET fusion detected” or “RET positive”.
If your colorectal cancer does not have a RET abnormality (RET negative, RET wild-type, RET non-mutant, or no RET gene fusion detected)
If your colorectal cancer has a RET abnormality (RET positive, RET mutant, or RET gene fusion detected)
While there are no current guidelines for RET testing in colorectal cancer, it should be considered in all patients with advanced or stage IV / metastatic colorectal cancer.
A biomarker is a piece of information about your health. Biomarkers include your blood pressure, your blood type, and cholesterol or blood sugar levels measured in a blood test. The biomarkers of cancer are also known as tumor markers.